Mild elevations in the liver enzymes alanine transaminase (ALT) and aspartate transaminase (AST) are commonly found in asymptomatic patients.
Mild elevations in the liver enzymes alanine transaminase (ALT) and aspartate transaminase (AST) are commonly found in asymptomatic patients.The most common cause is nonalcoholic fatty liver disease (sometimes called nonalcoholic steatohepatitis or NASH), which can affect up to 30% of the U.S. population.
Other common liver causes include:
- alcoholic liver disease
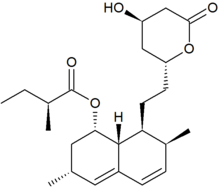
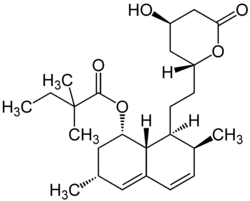
- medication-associated liver injury
- viral hepatitis (hepatitis B and C)
- hemochromatosis


Pale stool and dark urine (click to enlarge the images). This is an example of "obstructive" jaundice with the classic constellation of tea-colored urine and clay-colored stool.
Less common liver causes include:
- alpha-1-antitrypsin deficiency (AAT)
- autoimmune hepatitis
- Wilson disease
Extrahepatic conditions can also cause elevated liver transaminase levels:
- thyroid disorders
- celiac disease
- hemolysis
- muscle disorders
Initial testing should include:
- fasting lipid profile (FLP)
- measurement of glucose
- serum iron and ferritin; total iron-binding capacity (TIBC)
- hepatitis B surface antigen and hepatitis C virus antibody
If above test results are normal, a trial of lifestyle modification is appropriate.
Additional testing may include:
- ultrasonography (USG) of liver
- alpha-1-antitrypsin (AAT) and ceruloplasmin
- serum protein electrophoresis (SPEP)
- antinuclear antibody (ANA), smooth muscle antibody (ASMA), and liver/kidney microsomal antibody type
GI evaluation and possible liver biopsy is recommended if transaminase levels remain elevated for more than 6 months.
References:
Causes and evaluation of mildly elevated liver transaminase levels. Oh RC, Hustead TR. Am Fam Physician. 2011 Nov 1;84(9):1003-8.